
Part 4: The Broken Stick
Mary called to tell me that her beloved wooden-handled 20-year-old walking stick was broken.
Me: “Can it be fixed?”
Mary: “I’m afraid not”.
Me: “Did Dad take a look at it?”
Mary: Silence…
Me: “Are you sure?”
Mary: “Yes”.
She had already ventured out of her comfort zone to a local REI store and while they had similar Leki sticks, “they weren’t the same and wouldn’t do”. In retrospect, this may have been the turning point when she finally considered knee replacement. My father had been after her for 30-ish years and me about 20. Mary, who used to climb trees with me, was reduced to rollating and toddling on the furniture and countertops. From 3000 miles, it is difficult to give medical advice, but I tried. One of our home exchangers from New York had just undergone knee replacement at the renowned Hospital for Special Surgery in New York City. She had glowing recommendations for her surgeon and the hospital. She had done some serious research and considered her surgeon stellar, which my independent research corroborated.
There were two problems with the plan. First, Hospital for Special Surgery is in New York City and David just couldn’t be in the car that long. Secondly, being highly regarded, the doctor could not see her for 3 months, and while she had procrastinated for decades, this was too long to wait, now that she decided. She instead chose to go local. After all, David didn’t die at Hackensack Medical Center and it was only 45 minutes away. This was 15 minutes closer than the Hospital for Special Surgery and they didn’t have to pay a $13 toll! It was a win-win!
She consulted with the surgeon who “fixed” her back 20 years earlier. While semi-retired and not a knee surgeon, he gave her his unbiased opinion, suggesting a young colleague of his, Dr. Kissin. That was good enough for her and she soon had a surgery date. I tried to research Dr. Kissin, but to no avail. I at least found that he wasn’t on the folkloric surgeon shit list which all the prosthetic salesmen maintain. I begged Mary to reconsider and go to New York City for the procedure and she said she didn’t want some medical student doing her surgery. I assured her this was nonsense and that she could request the surgeon do the actual procedure, and not the orthopedic resident or fellow. She wasn’t having it. It was settled. Hackensack it was, and by the way, they have valet parking and soup in the cafeteria which David could eat.
(I embellished the logo ever so slightly)
She met with the surgeon, who made sure she had medical clearance. This is where she met Dr. Patel, an affable cardiologist she really liked. Some of her ‘numbers’ were a bit off, but there was no deal-breaker; nothing keeping her off the operating table. Mary shared her biggest concern, that she was chronically constipated. She was told “all old people are obsessed with their bowels and not to worry so much”.
With a date on the schedule, I imagined her with new knees at our Sedona, Arizona home, and while not hiking with us, enjoying the red rock mountain views from our patio. In this fantasy, David wasn’t alive, as he was 10 years older than she and would never agree to such a trip.
Friday before her surgery, Marie and I called her while stuck in Southern California rush hour traffic. The conversation went like this:
Me: “Hey M, ya’ know, I’m sure your surgery is going to go fine. It’s so routine these days, but I gotta ask… Do you have advanced directives? I assume D has power of attorney?”
Mary: “I’ve given this some thought. Do you have time now? Can you hear me OK? It sounds like you are underwater…”
Me: “I am underwater. It’s the fastest way home in traffic.”
Mary: “I didn’t get that…”
Me: “Yes, I mean no…I mean….go ahead…I can hear you just fine”.
Mary: “Well, you know I’m not looking forward to this…If things don’t go well. I mean if something doesn’t go well with anesthesia or something like that, I don’t want to be kept alive if I’m an invalid or brain damaged.”
Me: “So…”
Mary: “So if I’m too sick to ever get home and in a nursing home, I don’t want tubes…tube feedings and all. I wouldn’t want any of that. No life support and no CPR if that was the case.”
Me: “And…”
Mary: “But if I were a hopeless case, I want to be comfortable. I would want comfort care. I don’t want to be in pain. Do you know what I mean?”
Me: “Sure I do. I can definitely understand that. That’s true for both me and Marie. So D has power of attorney?”
Mary: “Yes”.
Me: “Have you discussed this with him…your preferences, I mean?”
Mary: “Yes”.
Me: “Does D understand?”
Mary: “I hope so. I think so. I think that he does”.
Me: “Do you have a hard copy of your advanced directives that you could send me?”
Mary: “We bought a will-maker at Costco about 10 years ago. I think I answered some questions about these things”.
Me: “Do you know where this is? Where the paperwork is?”
Mary: “No, but David might. I think it is on his computer or in his consultation room”.
Me: “ Oh God…that’s not good. Have you seen his office lately?”
Mary: “I know! Maybe you should ask him”.
That Sunday afternoon, I called David on his iPhone. The conversation went like this:
Me: “Hey D, it’s Steve. Howzit going?”
David: “Allllright…”
Me: “So, Hurricane Sandy is coming. Do you have enough duct tape?”
David: “Hmmm?”
Me: “Enough duct tape..duct tape”.
David: “What?”
Me: “Dad, could you put your hearing aides in? I want to talk to you about something”.
David: “Alright. Just give me a minute”.
Five minutes pass.
David: “What do you want to talk about?”
Me: “Mary, I wanted to talk about Mary”.
David: “What about?”
Me: “Well, about her knee surgery. I’m sure it will go well and all, but…well, did she talk to you about her advanced directives?”
David: “Advanced what?”.
Me: “Advanced DIRECTIVES…”
David: “Yeah”.
Me: “And?”
David: “And what?”
Me: “And are they clear? Do you know what she wants?”
David: “Yeah”.
Me: “And you’re OK with it?”
David: “OK with what?”
Me: “OK that she doesn’t want heroic measures?”
David: “Yeah”.
Me: “Yeah, what?”
David: “What?”
Me: “You understand her wishes?”
David: “Yeah”.
Me: “And?”
David: “And what?”
Me: “You are OK with it?”
David: “Your mother is depressed. She doesn’t know what she wants”.
Me: “She sounded pretty clear to me…”
David: “Yeah?”
Me: “Yeah, Dad. So you can honor her wishes? I mean, it’ll be fine and all, but if not. You’re OK with it?”
David: “Your mom’s a pessimist. She’s depressed”.
Me: “Wow, Dad, I don’t know…do you want to put her on the phone? I can call back on the house phone?”
David: “No”.
Hurricane (aka Superstorm) Sandy ravaged northern New Jersey and New York City on Monday October 29, 2012. The hospital was in an emergency mode, canceling all elective surgery, including Mary’s. Mary and David’s home was without power or water for several weeks. Services were eventually restored, but not before food in the deep freezers thawed. It seems the Costco generator was not up to the task. Apocalypse: 1 vs. 928: 0. Marie and I flew out later the week of Mary’s original surgery date. Our home exchange this time was deep in NOPO territory of the Upper West Side. (Manhattan was partially blacked out with a sharp line demarcating NOPO and SOPO, north or south of power).
( Manhattan after Superstorm Sandy showing NOPO and SOPO)
Mary’s new surgery date was moved a month back to December 3rd, 2012. Now properly bathed, she restocked the deep freezers with chicken pot pies from Costco, David’s favorite. She thought these would see him through her orthopedic rehabilitation.
As we biked to work that Monday, December 3rd, I chatted excitedly with Marie about what would be my mother’s new lease on life. This would be her year of rehabilitation, first the right knee, then the left. We would need to make a few more trips out to the east coast. Taking Mary out would likely be her only fun excursions as she took care of herself and David.
Accounting for the three hour time difference between New Jersey and California, I called Sarah after lunch, and was pleased to hear that Mary sailed through surgery and was only a bit goofy in the recovery room. Later that day, Mary and I had a brief chat on Sarah’s iPhone. Mary generally didn’t drink and I had never heard her slur her words before or nod off during a conversation. She survived surgery, was relatively comfortable and would soon be off to a skilled nursing facility, chosen by description, location and a brief field trip by Sarah, K and David.
Her three days on the orthopedic floor were reportedly uneventful, save one fall, on her way to the bathroom. Falls, infection, and bedsores should be rare occurrences at a good hospital. Two days is a typical stay, with a third day thrown in because of her age.
She was taken by ambulance to the nursing facility, which would be her home for the next several weeks, as she relearned how to get out of bed, walk the halls and use the bathroom. She lasted there only a few hours before becoming desperately ill with an overwhelming infection and dangerously low blood pressure. She was brought back by ambulance to Hackensack, but there were no beds available in the intensive care unit (ICU) where she belonged.
She was instead treated for two days in the emergency room on a small gurney in lieu of a proper hospital bed. Specialists on loan from the ICU looked in on her. With her blood pressure hovering dangerously low, Mary was plucked from the jaws of death long enough to get a CAT scan of her belly. Sarah or Susan called me with this update and my father warned me to come right away, as this might be the end for her. I managed to contact a sympathetic on-call radiologist, who gave me his opinion and electronic access to her CAT scan. He got it mostly right and together we surmised that she had rectal fecal impaction (severe constipation) which distended her colon to such a degree that blood flow was compromised, leading to what is called “ischemic bowel”.
Looking back, we can only surmise. Mary admitted to having a big problem with constipation and was reassured. She would not have been discharged from the hospital, if she had not moved her bowels. Perhaps she was on the honor system regarding bowel movements. Did she lie? My view from 3000 miles was that she was really distended on the CAT scan with what we call a drum belly. Discharging her in this condition, especially a post operative patient on narcotics, is really not good! There is a word for this and it starts with “m”.
Over the next two days, her blood pressure stabilized on pressors and her sepsis was treated. Her kidneys shut down from the low blood pressure, and her bowel was now bleeding. The fluid she received during her prolonged resuscitation caused her to bloat, with unrecognizable arms and legs. The excess fluid also expanded her new knee, leading the stitches to rip open. On top of this, she was so profoundly weak that she could not feed herself or brush her teeth. Getting into a chair was not possible. Rehabilitation was on hold indefinitely.
Various consultations were ordered. Infectious disease was happy with her antibiotics, orthopedics sent in a plastic surgeon to close her gaping surgical wound, gastroenterology confirmed ischemic colon and nephrology ordered a large bore catheter installed for hemodialysis. Her internist was the first to admit he was way out of his element with someone this sick, but reassured us that she was in good hands overall.
Stealing time from my workday, I spoke to one after another specialist. It wasn’t clear that they were coordinating her care, but hopefully at least were reading each other’s notes in her chart. She was started on hemodialysis and hated every second of it, from catheter pain, chest pain during the procedure, rigors, hypothermia and profound weakness. The nephrologist and her internist reassured us that her kidneys should kick back in soon and might not be much worse for wear if they did. If her renal function was going to recover, it would do so over a period of days to weeks, 6 weeks at the outside.
David called me tearfully at work on his iPhone.
David: “Stayven? You need to get out here. Your mother needs you. You’re the only one who can save her. You need to come out now”.
Me: “Dad, this is such a mess. I am so sorry! I don’t know what to say…I can try to get out in a week or so…there is no coverage for me!”
David: “Steven, this is your mother. She needs you. Her doctors are all idiots. You need to come out now. You are the only one who can save her”.
With these hopelessly unrealistic expectations, I called our executive assistant, Les, who arranged coverage for me the next week. I was able to get a room at the nearby Hasbrouck Hilton and flew out, hoping for some better news.
I made it to her room about 11:30 pm, armed with coffee and an iPad, in case Mary was asleep. She had a “deluxe” double room. Her roommate was an elderly Armenian woman who spent every waking minute coughing up green lumps mixed with lung tissue. I tentatively peeked around the curtain on Mary’s side of the room. Her arms, legs and abdomen were swollen, finger tips cracked. She looked pale and tired, but was awake. A slow embracing smile came across her face. Facial muscle wasting was already setting in from lack of eating and protein loss. While slightly alarming, she look younger than her 81 years.
A few minutes into our visit, a pained look came over her and she asked me to get the nurse, as she was too weak to find or even push the call button. She would have severe abdominal cramps from her bleeding bowel almost up until she died.
It was a short visit, as both of us were exhausted. I checked with Mary what time K and David visited and called Susan to see when she and Sarah would be out. Between Sarah and Susan, Mary had loving company most of the time.
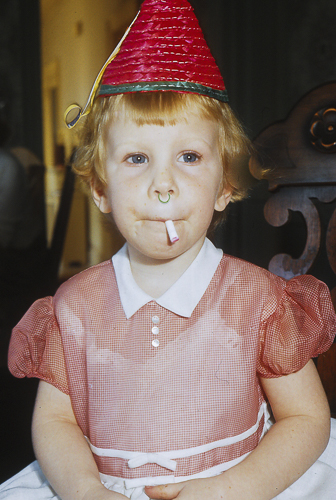
(Introducing Susan. She got her rebellious stage over early)
It is about a mile walk from the Hilton to the hospital through a blue collar neighborhood, gussied up with plastic Christmas dioramas and some left over Halloween decorations. Some silver tinsel was visible in the partially frozen sidewalk dog poop. The hospital had a cafe with passable scones and decent coffee. I made my way up to Mary’s floor and gently asked to see her chart and X rays, as well as the CAT scan.
Sarah and I both have medical backgrounds, but these doctors and nurses were not our colleagues. We were only visiting family and to hospital staff, family come in only a few flavors and styles. There is the mousy type, scurrying in and out with little fanfare. There are the sincere, who try their absolute best and follow all the rules. The takers eat their loved one’s food, watch what they want on the TV, and speak loudly on their cell phones, even when the medical team in the room. There is the Advocate, who writes everything and everyone’s names down. Then there is the coveted facilitator who brings pastries and chocolates for the staff, hoping to win favor. There is the dreaded toxic family that sucks the life out of the room and everyone they meet. Finally, there are the medical family members who second guess, and resent being on the outside. They can be extremely critical and can be frankly unpleasant.
 (My favorite picture of baby sister Sarah with her husband, Aaron)
(My favorite picture of baby sister Sarah with her husband, Aaron)
Of course, things are seldom completely black and white and mixtures of the above types can be found, sometimes even in the same individual. This is what we were. K was complementing aides on their bedpan skill and writing everything down. Sensing volatility, the staff was afraid of her. David was generally hostile and negative. Susan was present for most of Mary’s hospitalization and quietly attended to her needs. Sarah and I were trying to evaluate Mary’s care without being overly pushy, but speaking up when compelled. That said, my gentle pushing usually went nowhere. A CAT scan ordered in the morning might be completed by midnight, and we never got an air mattress or a quieter roommate for Mary.
Over the next few days, I met most of Mary’s attending physicians. Dr. Patel was her cardiologist and her de facto internist. On the good side, Mary lit up when he visited. He basically told me that he was way out of his element with her serious medical condition, but assured me of two things. First, that Mary’s kidneys would fire up sometime soon and second, the specialists looking after her were generally good. He was right about himself and the specialists, who individually seemed bright enough, but Mary didn’t fully benefit from the suboptimally coordinated care. The nephrologist corroborated that her renal function might recover. The gastroenterologist didn’t have much to say and I don’t think I met the infectious disease specialist. The orthopedic surgeon was attentive and came around to check on Mary’s now superfluous knee. He wanted to show me the postoperative X-rays of her knee. He was very proud of his work. I would have to agree, but Mary’s X-ray looked so much much better than she did. I sensed tremendous guilt and found myself actually trying to comfort him. I wondered if he would take constipation more seriously the next time.
Watching David and K attend to Mary was painful. Susan, being witness to this much more than me, recorded this journal entry:
“He comes into her room when she’s asleep or withdrawn deeply into herself and demands, “Mary! Mary! Mary!” and then seizes her hand and holds it so that her wrist bends backwards and hurts her. He pokes her repeatedly in the belly and hurts her. He fails to say he loves her when she says she loves him. (then) K tells her how much she has meant to her: she taught her to bleach her clothes with Clorox, and remember the time they were all in Israel and K and D went for a walk in Jerusalem”.
(David visiting Mary at Hackensack Medical Center)
David would go on about his remarkable phoenix-like ascent from death’s grasp and tried to give some well meaning tips. “…you gotta fight this,” and “Mary, squeeze my hand,” “Mary, eat your jello”. “Mary! Mary Mary!”
Fortunately, he would tire easily and go home. K would drop him home and often come back. She would sometimes read to Mary when she was having hemodialysis.
In spite of being a physician, I had never watched a dialysis session. Imagine a large room with multiple bays, mostly open to each other. While the machine was quiet, the procedure was not serene. Mary’s large dialysis catheter was finicky and caused her pain when in use. The procedure gave her shaking rigors and left her completely spent. She would be on dialysis three times a week, until her kidneys began working again. Each week, there were 3 shitty days, three less shitty days to recover and a seventh day to contemplate her existence.
Viewing her chart was a bit horrifying. Her nutritional status was in shambles. She was anemic with a high glucose and very low protein levels. The low protein was one of the reasons she was so swollen. She was also getting quite a few blood transfusions. Just to set the stage, my mother would balk at shaking hands with an obviously gay man and here she was getting loads of blood from strangers!
I asked the head nurse again for an air mattress as Mary was already getting “hot spots”, a precursor to bedsores. I also wanted her to have a nutrition consultation as she was wasting away. It seemed every other day, there was an NPO (nothing by mouth) order in anticipation of some procedure, which was often seriously delayed or even cancelled without explanation. When they did bring her food, it was often broth and dietetic green jello. The air mattress never arrived and the nutrition consultation consisted of a kitchen aide who asked if she liked chicken fingers and milk shakes. Her insulin schedule was horrible, but they still insisted on doing finger sticks around the clock. Care was generally too little and too late. So much for me saving the day and rescuing her. I wondered if Hurricane Sandy hadn’t happened and scuttled her house, would she have been so constipated? Did climate change kill my mother? I guess it may have, in the same way Hurricane Katrina killed people in Houston and Dallas who were victimized by a few low life refugees displaced from New Orleans.
Susan was at bedside for much of Mary’s hospital stays. She bought her an electric toothbrush, brushed her teeth and fed her homemade soup. She knitted her a throw and would read to her during dialysis. Sarah, a former hospice nurse, toted goodies, including coconut butter for Mary’s dry and chapped hands and an inflatable device for washing a bed-bound person’s hair. Mary was too weak to feed herself or brush her own teeth and with no experience being so dependent, relished the loving care from her daughters. With clean teeth and shiny red hair, her spirits were buoyed. Sarah’s husband, Aaron, visited as much as he could with Chopstick (their American bulldog) in the car. He was a great comfort to us all, with his broad infectious smile and optimism; I’m describing Aaron, not the dog. Chopstick would stay in the parking garage and while happy to do nothing, was always pleased to be taken for a walk around the block. She was our drooling, slack jowled therapy dog and knew it.





Incredible. I’m hooked!